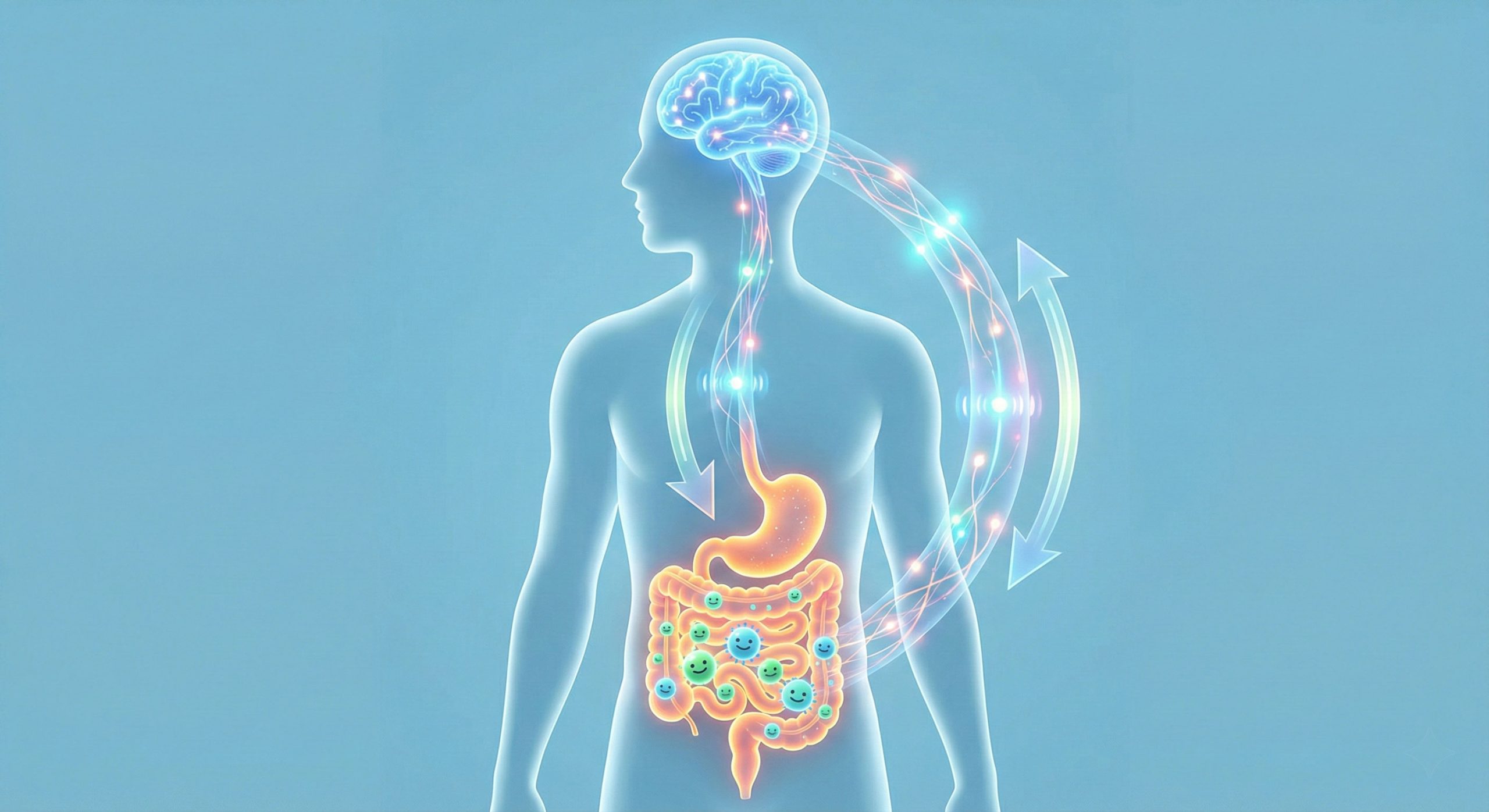
The connection between the gut and the brain has become a major area of interest in recent years. Many people notice changes in digestion when they feel stressed or shifts in mood when their digestive system feels unsettled. This two-way communication is known as the gut-brain axis, and it plays an important role in how the body regulates digestion, energy, mood, and general well-being.
Functional medicine explores these interactions in detail. By examining how different systems in the body influence one another, this approach helps people understand the factors affecting digestion, energy, and daily well-being. For many people living in Melbourne, these concerns often relate to lifestyle pressures, long workdays, or changes in routine. With this in mind, a functional medicine doctor in Melbourne can help identify patterns that contribute to how you feel and offer guidance that supports your care alongside your GP. This whole-system approach places emphasis on understanding how lifestyle, environment, and physiology interact.
How the Gut and Brain Communicate
The gut and the brain are constantly sending messages back and forth. This happens through several pathways, the most well-known being the vagus nerve, which acts like a communication highway between the digestive system and the central nervous system. Signals travel in both directions to help regulate hunger, satiety, digestion, and emotional responses.
Chemical messengers also play a role. The gut produces a range of neurotransmitters, including serotonin, which is often associated with mood regulation. While serotonin functions differently in the gut compared to the brain, its presence highlights how interconnected these systems are.
The immune system is another important pathway. Immune activity in the digestive tract can influence inflammation, which in turn may affect how the brain processes stress, energy, and mood. These interactions are complex, and research continues to evolve, but they form the foundation of what we refer to as the gut-brain axis.
The Role of the Gut Microbiome
The gut microbiome refers to the trillions of microorganisms that live in the digestive tract. These microbes help break down food, support nutrient absorption, produce certain vitamins, and interact with the immune system.
A balanced microbiome contributes to digestive comfort and general well-being. When the microbiome becomes disrupted, some people may experience changes in bowel habits, bloating, or fluctuations in energy and mood. Factors that may influence the microbiome include:
- diet low in fibre or whole foods
- high stress levels
- illness or infections
- medication use
- irregular sleep
- environmental exposures
Research into the microbiome is expanding rapidly. Scientists are still learning how specific bacteria interact with other systems in the body, and how lifestyle factors influence this balance. Functional medicine takes these connections into account when exploring a person’s overall health.
How Stress and Emotion Affect Digestion
Most people have experienced the feeling of an unsettled stomach during stressful moments. This happens because the nervous system responds to stress by shifting resources away from digestion and towards the body’s alert systems.
During periods of emotional strain or chronic stress, the digestive system may become more sensitive. People may notice:
- changes in appetite
- altered bowel habits
- increased digestive discomfort
- feelings of tightness or bloating
These responses are natural physiological reactions. Over time, ongoing stress can influence how the gut and brain communicate, reinforcing the importance of emotional well-being as part of digestive health.
How Digestive Health Can Influence Mood and Energy
The gut does not simply react to the brain; it also sends signals back that can influence mood, thinking, and energy levels. Nutrient absorption, inflammation, hormone regulation, and microbial balance all contribute to how the body feels throughout the day.
When digestion is not functioning optimally, some people may experience difficulty concentrating, reduced motivation, or a general sense of tiredness. These experiences vary widely and can be influenced by many factors, which is why a personalised approach is often helpful.
Functional Medicine’s Approach to Understanding the Gut-Brain Axis
Functional medicine takes a systems-based approach, meaning it examines how different parts of the body influence each other rather than viewing issues in isolation. When exploring the gut-brain axis, a functional medicine clinician will typically gather a detailed history to understand patterns that may be contributing to a person’s symptoms or concerns.
This may include discussing:
- current digestion and bowel habits
- dietary intake and eating patterns
- sleep quality and routine
- stress exposure at work, home, or emotionally
- physical activity
- environmental and lifestyle influences
By bringing these elements together, functional medicine aims to identify where support may be beneficial. This does not replace medical care; instead, it works alongside conventional treatment by highlighting lifestyle and environmental factors that influence health.
Assessment and Investigations in Functional Medicine
Assessment in functional medicine often involves a combination of medical history, physical health review, and, where appropriate, standard pathology tests arranged through a GP or medical practitioner. These may include blood tests that look at nutrient levels, markers of inflammation, thyroid function, or other metabolic indicators.
A practitioner may also explore digestive patterns, dietary triggers, bowel regularity, and stress-related changes. These assessments help build a holistic understanding of how the gut and brain may be influencing each other.
It is important to emphasise that testing is not used to diagnose mental health conditions or digestive diseases. Those conditions require conventional medical evaluation and, when needed, referral to specialist care.
Nutrition and Lifestyle Strategies That Support the Gut-Brain Axis
Lifestyle choices play a significant role in supporting both digestive health and emotional well-being. While individual needs vary, functional medicine often highlights general strategies that can be adapted based on personal circumstances. These may include:
- eating a varied, fibre-rich diet with plenty of whole foods
- drinking enough water throughout the day
- maintaining consistent sleep and wake times
- reducing excess caffeine or alcohol
- engaging in regular physical activity
These habits support the body’s ability to regulate energy, digestion, and mood in a balanced way. A practitioner can help tailor guidance to suit each person’s unique situation.
The Role of Stress Management in Gut-Brain Wellbeing
Because stress has such a strong influence on digestion and nervous system function, stress management is an important part of supporting the gut-brain axis. Gentle practices such as mindfulness, breathing exercises, yoga, or relaxation routines may help regulate the stress response and promote a sense of balance.
These approaches are not treatments for medical conditions, but they can complement medical care by supporting overall well-being and helping the body adapt to daily challenges.
Why Individualisation Matters in Functional Medicine
Everyone’s gut-brain axis works differently. Genetics, personal history, diet, lifestyle, emotional experiences, and environmental factors all influence how the gut and brain communicate.
Functional medicine emphasises individualisation because no single approach works for everyone. By understanding each person’s unique patterns, practitioners can offer guidance that aligns with their goals, preferences, and circumstances.
When to Seek Medical Review
Changes in digestion, mood, or energy levels should always be discussed with a GP, especially when symptoms persist or interfere with daily activities. Conditions such as coeliac disease, inflammatory bowel disease, thyroid disorders, anaemia, and other health issues require medical evaluation and appropriate treatment.
Functional medicine complements general practice by helping people explore lifestyle and environmental factors that may support their overall well-being. It does not replace medical care or specialist treatment.
FAQs
Q1: What is the gut-brain axis?
The gut-brain axis refers to the communication network between the digestive system and the nervous system, involving nerves, chemical messengers, and immune interactions.
Q2: Can digestive health affect mood?
Digestive function, nutrient absorption, and gut inflammation can influence how people feel day to day, although the relationship is complex and differs between individuals.
Q3: How does stress influence digestion?
Stress can affect appetite, motility, and digestive comfort by shifting the body into a state of heightened alertness, which reduces resources available for digestion.
Q4: What can functional medicine add to gut-brain support?
Functional medicine explores diet, sleep, stress, lifestyle, and medical history to understand how these factors influence the gut and brain together.
Q5: Should I see my GP about digestive or mood changes?
Yes. Persistent symptoms should always be reviewed by a doctor to rule out underlying health conditions and ensure appropriate care.
Disclaimer
This article is for general informational purposes only and does not replace professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider for guidance tailored to your personal circumstances.