Iron deficiency is one of the most common nutritional problems worldwide and can affect energy, concentration, and overall well-being. In Australia, treatment usually involves either oral iron supplements or iron infusions.
In major cities such as Melbourne, many patients who cannot tolerate tablets or who require quicker correction are referred for IV iron infusions where the treatment is delivered under medical supervision. Understanding how these options differ helps patients have informed discussions with their doctor about what might be appropriate for their situation.
How Iron Deficiency Is Diagnosed
Doctors typically arrange blood tests such as a full blood count, serum ferritin, and transferrin saturation to confirm iron deficiency. These results provide a clearer picture of iron stores and help determine whether treatment is required.
Identifying the underlying cause of low iron is also essential, whether it relates to diet, blood loss, or another health condition.
Why Iron Levels Drop
Iron deficiency can arise for many reasons. Common causes include inadequate intake from food, heavy menstrual bleeding, pregnancy, gastrointestinal blood loss, or reduced absorption due to conditions such as coeliac disease or following bariatric surgery.
In some cases, chronic illness contributes to falling levels. Replacing iron is important, but addressing the underlying cause is just as vital.
Oral Iron Supplements Explained
Oral iron is usually the first step in treatment. Tablets, capsules, and liquid preparations are available, with ferrous salts being the most commonly prescribed forms in Australia. They work by gradually increasing iron levels through absorption in the gut.
For best results, oral iron is often taken on an empty stomach with water. Some drinks, such as tea or coffee, can reduce absorption, while vitamin C may improve it. Gastrointestinal side effects such as constipation, nausea, or dark stools are common, though these can sometimes be reduced by adjusting the dose or trying a different preparation.
Oral supplements are generally most suitable for mild to moderate deficiency, provided the patient can tolerate them.
Iron Infusions Explained
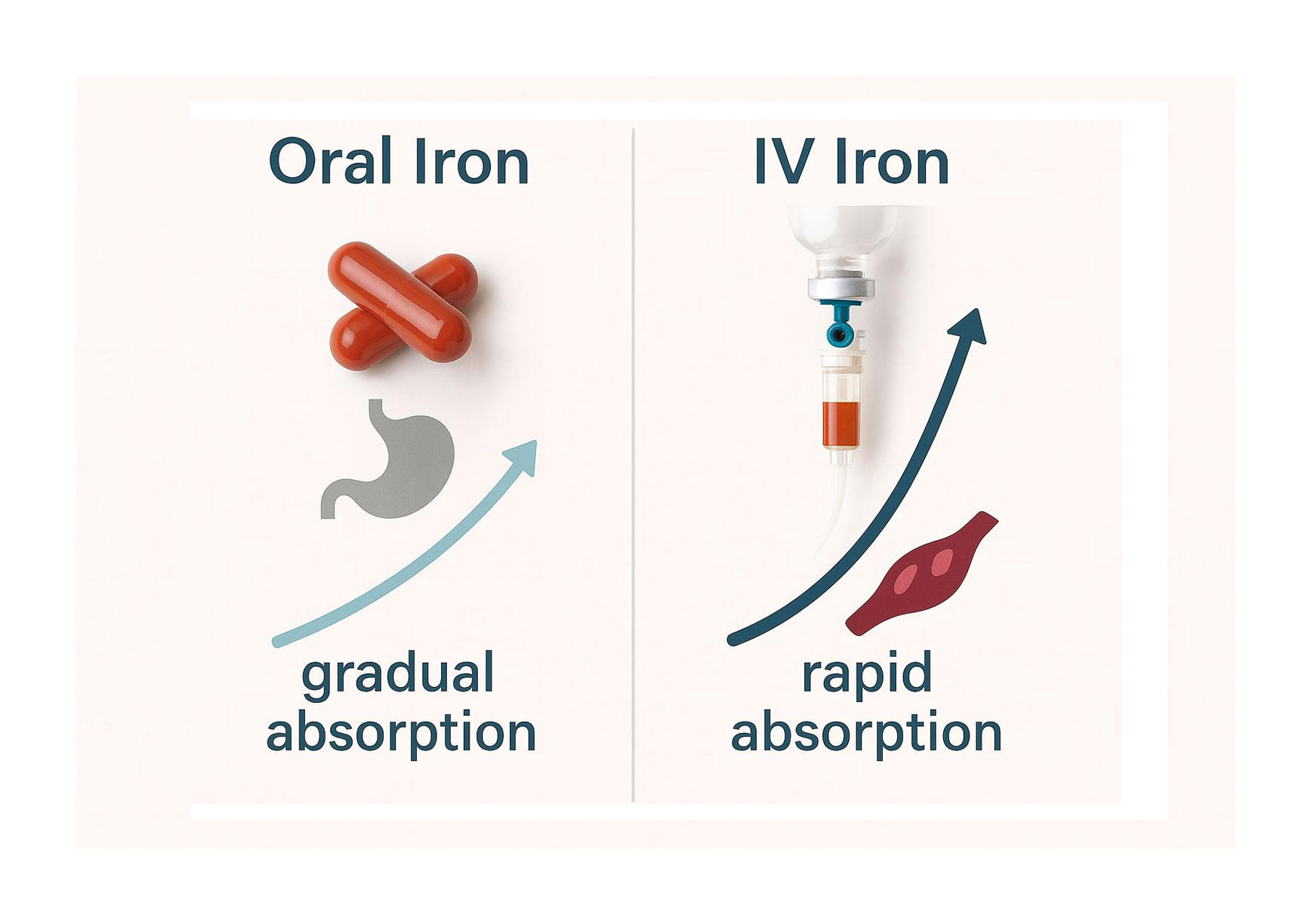
An iron infusion is a procedure where iron is delivered directly into the bloodstream through a drip. This bypasses the digestive system and allows for faster replenishment of iron stores.
During an infusion, a cannula is inserted into a vein and the solution is administered under supervision. The process usually takes 30 to 60 minutes, followed by a period of observation to monitor for any reaction.
One or two sessions are often enough to correct deficiency, though follow-up testing is still required. Infusions may be recommended when oral iron is not effective, not tolerated, or when deficiency is more severe.
Safety and Side Effects
All treatments have possible side effects. Oral iron can cause stomach upset, constipation, or staining of teeth with liquid forms. For many people, these issues improve with dose adjustments or switching brands.
Iron infusions are generally well tolerated but can occasionally cause flu-like symptoms, headache, or dizziness shortly after treatment. Rarely, more serious allergic reactions can occur, which is why the procedure is carried out in a clinical setting.
A small risk of skin staining exists if iron leaks outside the vein. Monitoring and follow up with a doctor are important to ensure safety.
Diet and Absorption Support
Food remains an important source of iron. Lean red meat, chicken, seafood, legumes, leafy green vegetables, and fortified cereals contribute to iron intake.
Combining plant-based sources with vitamin C-rich foods, such as fruit or capsicum, can improve absorption. While diet alone may not correct significant deficiency, it plays a supportive role alongside supplements or infusions.
Comparing Oral Supplements and Infusions
The main difference lies in speed and tolerability. Oral iron gradually improves levels over weeks to months, provided it is taken consistently. Iron infusions deliver a more rapid rise, which may be crucial in certain situations such as late pregnancy or after major blood loss.
Convenience also differs. Oral iron can be taken at home but requires ongoing daily commitment. Infusions require a clinic visit but may reduce the need for long-term tablets. Cost, availability, and individual preference also factor into decision-making.
Special Situations
Pregnancy increases the body’s iron requirements. While oral supplements are often used, infusions may be considered later in pregnancy if levels remain low despite tablets.
In chronic kidney disease, infusions are sometimes integrated into broader treatment plans. Patients who have undergone bariatric surgery may also require infusions due to absorption difficulties. In each case, the decision is tailored to individual needs.
Monitoring and Follow-up
After starting treatment, doctors usually recheck blood tests within a few months to assess progress. If levels return to normal, oral iron may continue for a time to replenish stores fully.
Regular monitoring prevents both under-treatment and excess iron, ensuring care remains safe and effective.
Choosing the Right Option with Your Doctor
No single treatment suits everyone. A doctor considers test results, symptoms, medical history, and response to past treatment when recommending oral supplements or infusions.
Personal preference also plays a role, but medical guidance is central to choosing the safest and most effective option.
FAQs
Q1: Do I need tests before starting iron tablets or an infusion
A1: Yes. Blood tests are usually required to confirm iron deficiency and guide treatment decisions.
Q2: How soon might I notice changes after an infusion or with tablets
A2: With tablets, improvement may take several weeks. Infusions can restore iron more quickly, though symptom relief still varies from person to person.
Q3: Can I switch from tablets to an infusion if I feel unwell on tablets
A3: In some cases, yes. If side effects are problematic or tablets are not effective, a doctor may recommend an infusion.
Q4: Is an iron infusion suitable during pregnancy
A4: Oral iron is usually the first choice. Infusions may be considered in later stages if deficiency is significant and tablets are not sufficient.
Q5: Can I keep taking oral iron after an infusion
A5: Sometimes ongoing tablets are prescribed to maintain levels, but this depends on individual needs and should be guided by a doctor.
Q6: Can I drive home after an infusion
A6: Most people can, although clinics may recommend arranging transport if you feel unwell during or after treatment.
Q7: How often will my levels be checked
A7: Follow-up blood tests are usually carried out a few months after starting or completing treatment, with ongoing monitoring if needed.
Disclaimer
This information is provided for educational purposes only and is not a substitute for professional medical advice. Always seek the guidance of a qualified health professional with any questions you may have regarding your health or treatment options.