Diabetes is one of the most common long-term conditions affecting Australians today. Managing blood sugar is central to protecting health, yet every person’s experience of diabetes is unique. Functional medicine looks beyond a one-size-fits-all approach and emphasises the underlying factors that influence health.
By addressing nutrition, movement, sleep, and stress alongside standard medical care, it aims to create a personalised plan that supports both blood sugar control and overall wellbeing.
In Australia, some people with diabetes also experience iron deficiency, which may require treatment beyond diet and supplements. For those situations, medical iron infusions in Melbourne can be provided under specialist supervision to restore iron levels and support overall health.
Understanding Diabetes
There are several types of diabetes. Type 1 diabetes occurs when the body cannot produce insulin and requires lifelong insulin therapy. Type 2 diabetes, which is more common, arises when the body becomes resistant to insulin or produces it in insufficient amounts. Gestational diabetes develops during pregnancy and usually resolves after birth, though it can increase the risk of later type 2 diabetes.
Whatever the type, the principle remains the same: blood glucose levels need to be managed to prevent both day-to-day symptoms and long-term complications. Conventional care focuses on medication, blood glucose monitoring, and lifestyle guidance from health professionals. Functional medicine builds on this by asking: what factors are driving imbalance, and how can they be improved?
What Functional Medicine Involves
Functional medicine is based on a whole-person approach. It begins with a detailed history, not only of medical conditions but also diet, physical activity, stress levels, sleep, and environmental influences. The aim is to identify patterns that might be contributing to poor blood glucose control.
Treatment plans are then tailored, often combining nutritional strategies, exercise, stress reduction, and sleep routines with conventional medical therapy. Importantly, functional medicine does not replace prescribed diabetes care; instead, it complements it through personalisation.
Root Causes and Contributing Factors
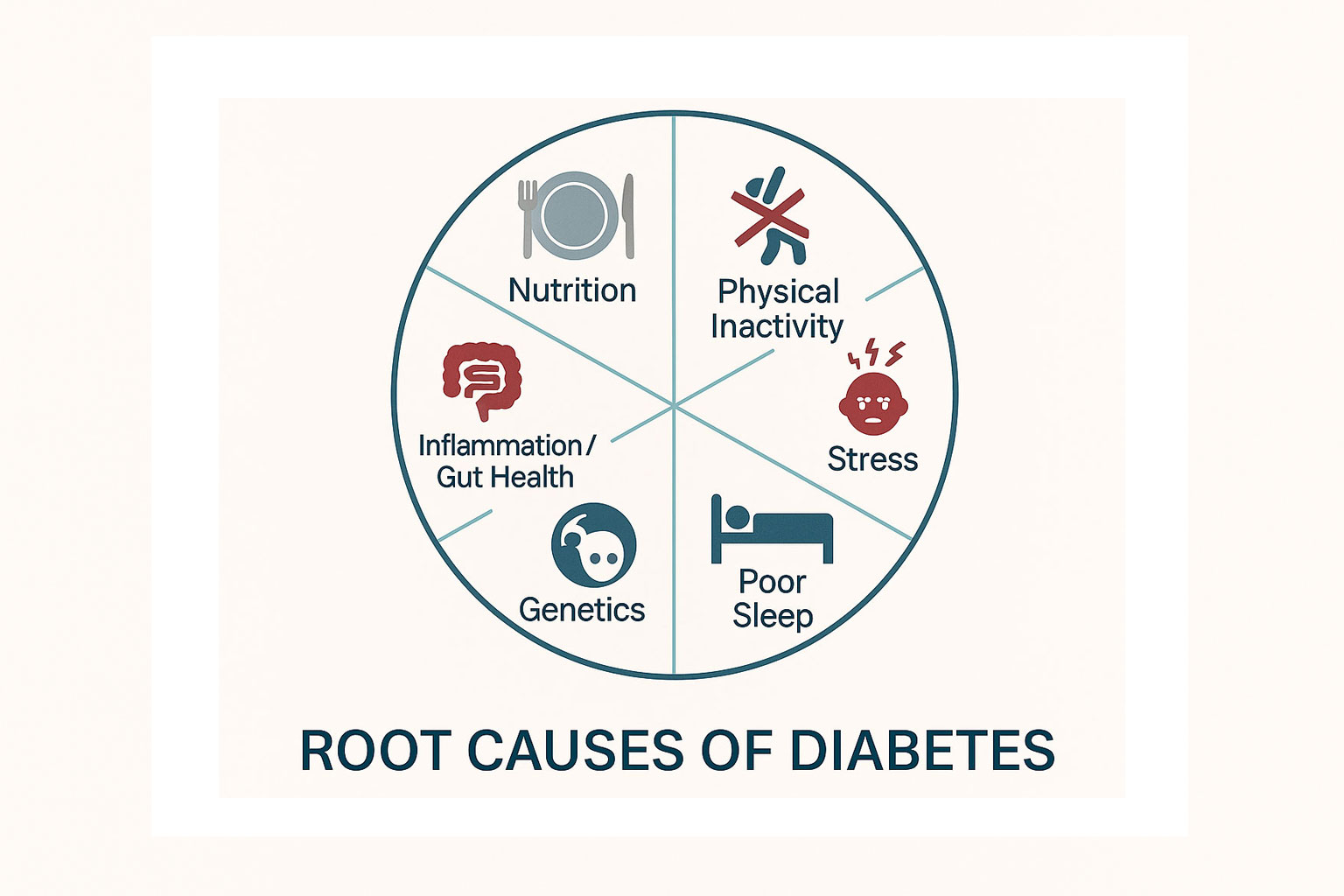
Diabetes does not usually stem from a single cause. Functional medicine considers the combined effect of several contributors:
- Nutrition patterns high in refined carbohydrates or lacking fibre.
- Sedentary lifestyle or insufficient physical activity.
- Stress and poor sleep disrupting hormones that affect glucose balance.
- Family history or genetic factors that increase risk.
- Inflammation and gut health issues that may influence metabolism.
Looking at these influences helps create a clearer picture of what may be driving an individual’s condition.
Nutrition Foundations for Glycaemic Control
Diet is central to managing diabetes. Functional medicine emphasises a balanced plate with:
- Fibre-rich carbohydrates such as vegetables, legumes, and whole grains.
- Lean protein sources to aid satiety and stabilise blood sugar.
- Healthy fats like olive oil, avocado, and nuts.
Meal timing can also influence blood sugar, and spacing protein throughout the day helps maintain energy and prevent spikes. Adjustments are tailored to cultural food preferences, budget, and tolerance. For example, pairing plant-based iron sources with vitamin C-rich foods can improve absorption and support those following vegetarian diets.
Lifestyle Interventions That Support Insulin Sensitivity
Lifestyle changes work alongside diet to improve how the body responds to insulin. Regular movement, from walking to strength training, increases glucose uptake by muscles and improves sensitivity.
Sleep is equally important; disrupted or insufficient sleep can worsen insulin resistance. Stress management techniques, even brief pauses for breathing exercises or short walks, may help stabilise cortisol levels, which in turn influence blood sugar.
Functional Medicine Assessment and Testing
A thorough assessment in functional medicine covers both conventional and broader markers. Doctors may request:
- HbA1c to track average blood glucose over several months.
- Fasting and post-meal glucose checks.
- Lipid profiles, kidney and liver function tests.
- Inflammatory markers if indicated.
Some patients may use continuous glucose monitoring, which provides detailed feedback on daily fluctuations. This data helps shape individual recommendations.
Monitoring and Treatment Targets
Functional medicine does not replace clinical targets but works alongside them. Most patients will have an HbA1c goal set by their treating doctor. Fasting and post-meal glucose ranges are also personalised.
Progress is reviewed regularly, with goals adjusted as health changes. This ongoing monitoring ensures safety and provides accountability.
Integrating Medications with Functional Care
Medications remain central to diabetes management. Metformin, GLP-1 receptor agonists, and insulin are common treatments. Functional strategies are designed to complement these medicines, not replace them.
Coordination with a GP or endocrinologist is essential, particularly to avoid risks such as hypoglycaemia when diet or activity changes are introduced.
Weight, Insulin Resistance, and Body Composition
For many people with type 2 diabetes, excess weight and insulin resistance are closely linked. Functional medicine highlights gradual, sustainable weight reduction where appropriate.
Resistance training helps preserve muscle mass, which in turn supports glucose use. Distributing protein evenly across meals can also assist in appetite control and metabolic stability. Even modest changes in weight may improve insulin action and lower glucose levels.
Complication Risk Reduction
Diabetes increases the risk of heart, kidney, nerve, and eye conditions. Functional medicine addresses these risks by supporting modifiable factors: maintaining healthy blood pressure, improving lipid profiles, and encouraging routine screenings.
Eye checks and foot care are important for early detection of complications. Stopping smoking and moderating alcohol intake, when relevant, further reduce risk.
Supplements And Adjunct Therapies
Some functional medicine practitioners consider supplements, such as specific vitamins or minerals, but only when clinically indicated.
Caution is required, as supplements can interact with prescribed medicines or be unnecessary. Any supplement plan should be guided by a qualified clinician.
Life Stages and Special Situations
Functional medicine adapts care to different life stages:
- Pregnancy: managing gestational diabetes safely with input from obstetric and diabetes teams.
- Adolescents: supporting families to build healthy habits during growth.
- Older adults: focusing on fall prevention, cognitive support, and comorbidities.
- Shift workers: developing practical strategies to stabilise glucose with irregular meal and sleep times.
Mental Health and Behaviour Support
Diabetes can affect mood and motivation. Functional medicine recognises this link and incorporates support for mental well-being. Approaches may include brief counselling strategies, stress reduction techniques, and encouragement of social or peer support. Small, achievable changes are emphasised to build confidence and reduce distress.
Safety and Red Flags
Safety is a central part of any care plan. Patients are advised to seek urgent review for symptoms of very high or very low blood sugar, such as confusion, dizziness, or loss of consciousness.
Sick-day management, including adjusting treatment during illness, is discussed with a doctor. Functional medicine reinforces that prescribed medication should never be altered without professional advice.
Building a Personal Care Plan
A key feature of functional medicine is setting manageable goals. This often means starting with one or two changes at a time, such as walking after meals or improving sleep routines. Goals are specific, measurable, and reviewed regularly. This structured approach allows progress to be tracked and adjusted as needed.
When To Seek Medical Advice
Anyone experiencing new or worsening symptoms, such as persistent fatigue, unexplained weight loss, or frequent infections, should seek prompt medical review. Regular check-ups and screenings remain essential, even when making lifestyle improvements. Professional oversight ensures care is both safe and effective.
FAQs
Q1: What makes functional medicine different in diabetes care?
A1: Functional medicine looks at root causes and lifestyle influences while still supporting conventional medical care.
Q2: Can a functional approach reduce the need for medication?
A2: In some cases, lifestyle changes may reduce medication requirements, but the treating doctor must always make this decision.
Q3: Which tests are used and how often are they repeated?
A3: Common tests include HbA1c, fasting glucose, and lipids. Frequency depends on individual care plans and medical advice.
Q4: How do movement and sleep affect blood glucose?
A4: Regular activity improves insulin sensitivity, while good sleep supports hormone balance. Both help stabilise blood sugar.
Q5: Is a functional approach suitable for type 1 diabetes?
A5: Functional strategies may support overall well-being, but insulin remains essential. Any changes should be coordinated with a specialist.
Disclaimer
This information is provided for general education and is not a substitute for professional medical advice. Always seek the guidance of a qualified healthcare professional for diagnosis and treatment tailored to your individual needs.