Iron plays an essential role in supporting oxygen transport, energy production, cognitive clarity, and immune function. When levels fall, people may begin to feel unusually tired, light-headed, low in mood, or short of breath. Iron deficiency is common in Australia, and oral iron supplements are often used as a first step in treatment. However, not everyone absorbs oral iron well, and some people find that supplements cause digestive discomfort or fail to improve their iron levels.
Many people in Melbourne seek support when low iron affects their energy, concentration, or daily routine, especially if they have had difficulty improving their levels with dietary changes alone. For individuals who need another option, iron infusions in Melbourne may be considered when oral iron is not suitable, not tolerated, or not effective. Understanding how gut health influences iron absorption can help explain why treatment responses vary from person to person and why some people benefit from medical review to explore the most appropriate approach.
How the Gut Absorbs Iron
Iron absorption occurs primarily in the small intestine, where the digestive system breaks down dietary iron into forms the body can use. There are two types of dietary iron:
- haem iron, found in animal foods and generally easier for the body to absorb
- non-haem iron, found in plant foods and more affected by other dietary factors
For absorption to occur, the stomach must produce adequate acid to convert iron into a usable form. The small intestine then transports the iron through specialised cells, where it enters the bloodstream and is stored for later use.
The process is influenced by many factors, including overall gut function, diet, inflammation, and certain medications. Vitamin C, for example, can support absorption, while substances like tannins (found in tea and coffee), phytates (in some grains and legumes), and calcium can reduce it. Because this system is so sensitive, even small changes in digestive health can make a noticeable difference to how the body handles iron.
Common Gut-Related Reasons Oral Iron Supplements May Not Work Well
Oral iron relies entirely on the digestive system, and many people experience challenges that make supplements difficult to tolerate or poorly absorbed. Several gut-related issues can contribute to reduced effectiveness.
- Gastrointestinal conditions that reduce absorption
Some medical conditions affect the lining of the stomach or small intestine, interfering with the body’s ability to take in nutrients. These may include:
- coeliac disease
- inflammatory bowel disease
- atrophic gastritis
- Helicobacter pylori infection
In these situations, iron may pass through the digestive tract without being absorbed effectively. Medical assessment is essential to identify these conditions and ensure the most suitable treatment plan.
- Reduced stomach acid
Iron needs adequate stomach acid for proper breakdown. Lower acid levels may occur due to:
- long-term proton pump inhibitor (PPI) use
- age-related changes
- chronic stress
When acid levels fall, iron may not convert into an absorbable form, reducing the effectiveness of oral supplements.
- Dietary factors or digestive patterns affecting absorption
Some people experience ongoing bloating, inflammation, or irregular digestion that interferes with nutrient uptake. Others follow dietary patterns that unintentionally hinder absorption, such as drinking tea or coffee close to mealtimes or consuming foods that reduce iron availability.
- Side effects leading to poor adherence
Iron tablets can cause gastrointestinal discomfort for some people, including:
- nausea
- constipation
- abdominal cramping
- metallic taste
These symptoms can make it difficult to continue taking oral iron long enough for levels to improve. Stopping supplements early often results in limited progress and lingering symptoms of low iron.
These issues highlight why iron deficiency should always be assessed by a GP, rather than managed through self-diagnosis or over-the-counter supplements.
How Inflammation and Gut Health Influence Iron Levels
Many people are surprised to learn that inflammation can directly affect iron absorption. When the body detects inflammation, it increases production of a hormone called hepcidin, which blocks iron from entering the bloodstream. This protective mechanism is designed to restrict iron availability during illness, but in chronic inflammatory conditions, it can contribute to low iron levels.
This can lead to a situation called functional iron deficiency, where the body has iron stores but cannot use them effectively. In these cases, oral iron supplementation may not work well because the body continues to block absorption.
Inflammation may arise from infections, autoimmune conditions, gut disorders, stress, or other chronic health concerns. Medical testing is needed to determine whether inflammation is playing a role.
The Role of Iron Infusions When Oral Iron Is Not Suitable
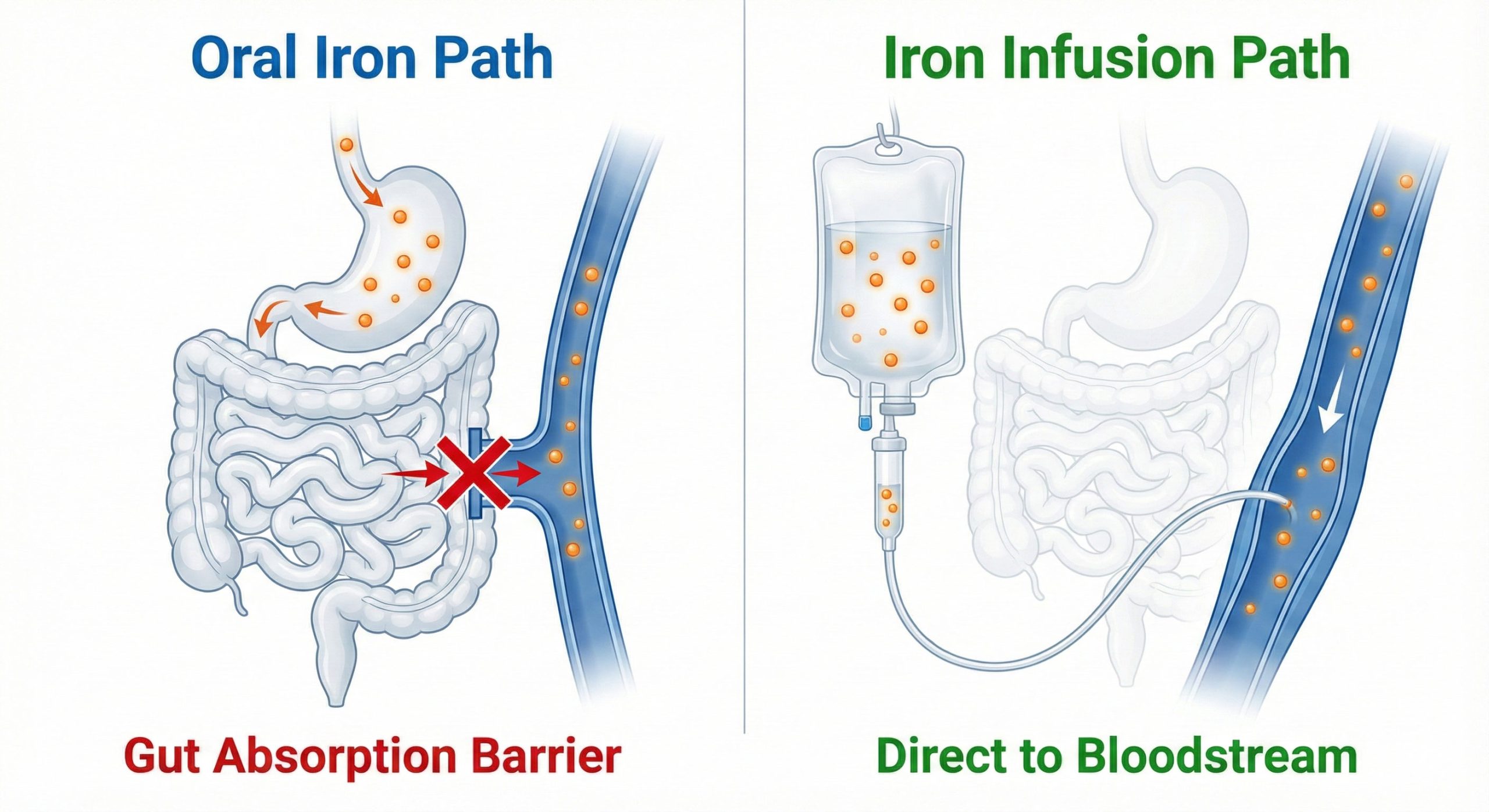
When oral iron is not effective or not tolerated, iron infusions may be considered as part of a medically supervised treatment plan. An iron infusion delivers iron directly into the bloodstream, bypassing the digestive system entirely. This makes infusions a helpful option for people who:
- cannot absorb iron due to gut-related conditions
- have persistent side effects from oral tablets
- require faster repletion in medically appropriate circumstances
- have iron deficiency linked to chronic inflammation
An infusion can only be recommended after proper medical review, including blood tests and assessment of symptoms and health history. It is not a general wellness treatment and should not be used without clinical justification.
Symptoms That May Suggest Oral Iron Is Not Effective
Individuals may begin to suspect that oral iron is not working well if they experience persistent symptoms despite following medical guidance. These may include:
- ongoing fatigue
- breathlessness on exertion
- reduced concentration or cognitive fog
- frequent dizziness
- digestive discomfort from supplements
- minimal improvement after a medically appropriate trial of oral iron
These signs can have many causes, so professional evaluation is essential. A GP can review symptoms, order blood tests, and determine the most suitable approach.
Why Individual Assessment Matters
Iron deficiency can arise from many different circumstances, including inadequate intake, menstrual blood loss, pregnancy, chronic illness, digestive conditions, or reduced absorption. Because the causes are so varied, treatment must always be personalised.
Some people respond well to dietary changes and oral supplements. Others require investigation for underlying causes or may be candidates for iron infusion therapy under medical supervision. A thorough assessment ensures that treatment is safe, appropriate, and tailored to individual needs.
Supporting Gut Health to Improve Iron Absorption
Many daily habits influence digestion and nutrient absorption. While lifestyle changes alone cannot correct iron deficiency, supporting gut health may complement medical treatment. Some general well-being strategies include:
- choosing a diet that emphasises whole foods and fibre
- drinking adequate water throughout the day
- minimising excess caffeine and alcohol
- establishing consistent sleep routines
- addressing digestive symptoms early with a healthcare professional
These approaches are not substitutes for medical care but can help create a healthier foundation for the body’s natural processes.
How Holistic and Functional Approaches Complement Medical Care
Holistic and functional medicine perspectives may explore nutrition, stress management, sleep, and lifestyle patterns that influence gut health. These approaches work alongside conventional medical treatment by encouraging a broader understanding of the factors affecting wellbeing.
They do not replace iron supplementation, oral medication, or iron infusion therapy when it is clinically appropriate. Instead, they can complement medical care by helping individuals establish supportive habits that contribute to long-term health.
When to Seek Medical Review
Professional assessment is essential when experiencing symptoms that could indicate iron deficiency or when oral supplements are not helping. You should seek medical review if you notice:
- persistent tiredness
- breathlessness
- worsening symptoms
- difficulty tolerating oral iron
- little or no improvement after a prescribed course
- ongoing digestive issues
- unexplained bleeding
A GP can organise the necessary blood tests and provide guidance on the next steps. Early evaluation can help prevent symptoms from worsening and ensure you receive safe, appropriate care.
FAQs
Q1: Why do some people struggle with oral iron supplements?
Absorption depends on gut function, stomach acid, inflammation, and overall digestive health. Some people also experience side effects that make consistent use difficult.
Q2: Are iron infusions more effective than oral iron?
Effectiveness depends on individual circumstances. Infusions may be considered when oral iron is not suitable, not tolerated, or not effective, and only after medical assessment.
Q3: Can improving gut health help with iron levels?
General gut wellbeing may support nutrient absorption, but low iron requires proper diagnosis and medical supervision.
Q4: How do doctors decide between oral iron and an iron infusion?
A GP considers blood test results, symptoms, medical history, and whether oral iron has been effective or tolerated.
Q5: Is it safe to take over-the-counter iron supplements without medical advice?
Iron supplements can cause harm if taken unnecessarily. They should only be used under medical supervision.
Disclaimer
This article is for general informational purposes only and does not replace professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider for personalised guidance.