Fatigue is something most people experience at some point, often linked to busy schedules, disrupted sleep, or short periods of stress. For some, however, fatigue does not resolve with rest and continues over time. Ongoing fatigue can affect how a person functions day to day and may feel difficult to explain or address. In Australia, including across Victoria, many people look for broader ways to understand why fatigue persists and how it fits into their overall health picture.
Functional medicine approaches persistent fatigue by recognising that it is rarely linked to a single factor. Rather than focusing on quick fixes, this perspective aims to understand the broader context in which fatigue occurs, including lifestyle demands, physical health, and emotional well-being. For those seeking care from a functional medicine doctor in Melbourne, this often means taking the time to explore how different aspects of health interact rather than viewing fatigue in isolation.
Understanding Fatigue That Persists Over Time
Fatigue that persists over weeks or months can feel very different from ordinary tiredness. People often describe a sense of low energy that does not improve even after sleep or time off. This type of fatigue may affect motivation, focus, and the ability to manage everyday tasks.
It is important to recognise that persistent fatigue is a common experience and can arise for many reasons. The way fatigue is felt and described varies widely, which is why it can be challenging to understand or manage without a broader health context.
What Is Meant by Chronic Fatigue Symptoms
The term chronic fatigue symptoms is often used to describe fatigue that lingers and interferes with daily life. This does not refer to a specific diagnosis but rather to an ongoing experience of low energy that feels out of proportion to activity levels or rest.
People may describe feeling physically drained, mentally foggy, or unable to sustain energy throughout the day. These experiences can fluctuate, sometimes improving briefly before returning. Focusing on symptoms rather than labels allows for a more flexible and individual approach.
How Fatigue Can Affect Daily Functioning
Ongoing fatigue can influence many aspects of daily life. Concentration and memory may feel reduced, making work or study more challenging. Physical tasks may require greater effort, and motivation can decline when energy feels limited.
Fatigue can also affect social interactions and personal routines. Over time, this can lead to frustration or a sense of being disconnected from usual activities. Acknowledging the real impact of fatigue is an important part of understanding its role in overall wellbeing.
Why Chronic Fatigue Symptoms Can Be Complex
Persistent fatigue is rarely linked to a single cause. Physical health, emotional stress, sleep patterns, nutrition, and daily demands often interact in ways that influence energy levels. Addressing one factor alone may not lead to meaningful change if other contributors remain unaddressed.
Functional medicine views fatigue as a complex experience shaped by multiple systems rather than an isolated issue. This perspective helps explain why fatigue can feel difficult to resolve and why experiences differ so widely between individuals.
The Functional Medicine Perspective on Fatigue
Functional medicine focuses on understanding patterns and relationships within the body rather than isolating symptoms. When applied to fatigue, this means considering how different systems may influence energy over time.
Rather than assuming a single explanation, functional medicine recognises individual variation and looks at how lifestyle, health history, and current stressors interact. This approach is educational in nature and does not replace medical assessment or diagnosis.
Common Contributors Explored in Functional Medicine
When exploring fatigue, functional medicine often considers a range of factors that may influence energy levels. These are viewed as potential contributors rather than direct causes.
Sleep quality and recovery patterns can play a role, particularly when sleep is disrupted or inconsistent. Nutritional intake may influence energy availability, especially when meals are irregular or poorly tolerated. Stress load and nervous system demands can also affect how the body uses and restores energy.
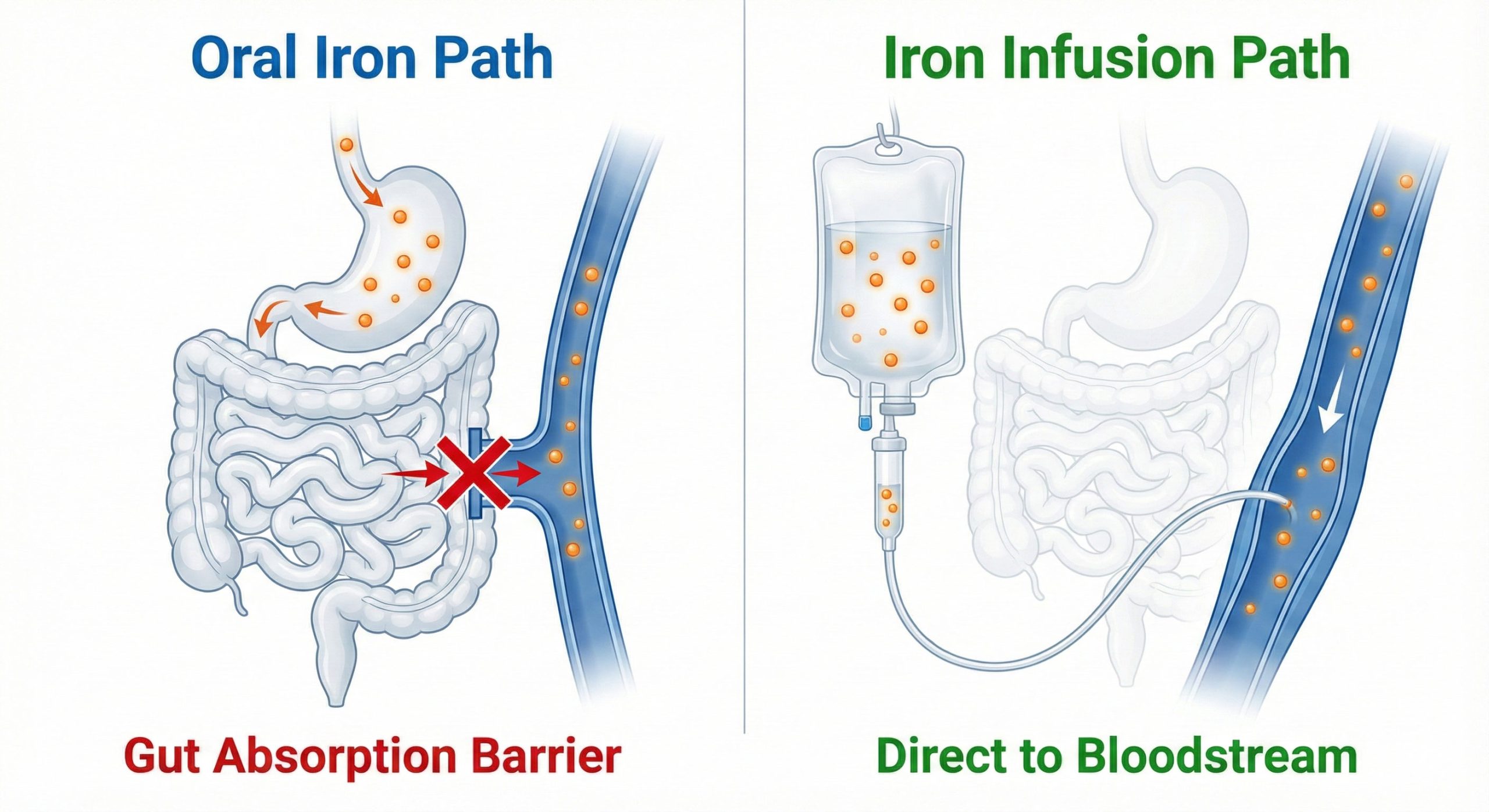
Physical activity levels are considered in relation to recovery rather than performance alone. Digestive function and nutrient absorption may also be explored as part of a broader picture, particularly when fatigue is accompanied by other symptoms.
The Role of Lifestyle Demands in Ongoing Fatigue
Modern lifestyles often place sustained demands on attention and energy. Long work hours, constant connectivity, and limited recovery time can contribute to cumulative fatigue over time.
Even when sleep duration appears adequate, ongoing mental load and reduced opportunities for rest can influence how refreshed a person feels. Functional medicine places emphasis on understanding these demands without assigning blame or oversimplifying their impact.
Energy Fluctuations and Nonlinear Recovery
Energy levels do not always improve in a steady or predictable way. Many people experience fluctuations, with days of improved energy followed by periods of increased fatigue.
Understanding recovery as non-linear can help reduce frustration and unrealistic expectations. Pacing activities and recognising early signs of fatigue are often discussed as ways to support daily functioning rather than pushing through low energy.
How Functional Medicine Supports Understanding Fatigue Symptoms
Functional medicine supports understanding fatigue by gathering a detailed picture of an individual’s health and lifestyle. This includes looking at current routines, stressors, sleep patterns, and personal health history together rather than in isolation.
The focus is on individual context rather than standardised pathways. This approach is intended to complement, not replace, conventional medical care and encourages collaboration with qualified healthcare professionals.
When Ongoing Fatigue May Warrant Further Discussion
Persistent fatigue that affects quality of life may benefit from further discussion with a healthcare professional. Difficulty managing daily responsibilities, ongoing low energy, or concerns about overall well-being can be reasons to seek guidance.
Early conversations can help clarify what support may be appropriate and provide reassurance where needed. Seeking advice does not require symptoms to reach a specific threshold and can be part of proactive health care.
FAQs
Q1: What is the difference between tiredness and chronic fatigue symptoms?
A1: Tiredness is often temporary and linked to activity or short-term stress. Chronic fatigue symptoms describe fatigue that persists over time and affects daily functioning, even with rest.
Q2: Can stress alone cause ongoing fatigue?
A2: Stress can contribute to fatigue, but it is often one of several factors. Lifestyle demands, sleep patterns, and physical health may also play a role.
Q3: Does functional medicine diagnose chronic fatigue conditions?
A3: Functional medicine does not replace medical diagnosis. It focuses on understanding patterns and supporting overall health alongside standard medical care.
Q4: Why does fatigue sometimes persist even with adequate sleep?
A4: Sleep duration is only one part of recovery. Stress, nutrition, lifestyle demands, and individual health factors can influence how restorative sleep feels.
Q5: When should someone seek professional advice for ongoing fatigue?
A5: If fatigue persists, affects quality of life, or feels difficult to manage, speaking with a qualified healthcare professional is recommended.
Disclaimer
This article is provided for general informational purposes only and does not replace personalised medical advice. Individual health needs vary, and readers are encouraged to consult a qualified healthcare professional for guidance relevant to their situation.